Barometric pressure changes can significantly affect both Mast Cell Activation Syndrome (MCAS) and dysautonomia due to the body’s sensitivity to environmental changes. Here’s how:
Effects on Mast Cell Activation Syndrome (MCAS):
- Mast Cell Degranulation: Barometric pressure changes, particularly drops, can trigger mast cells to release mediators like histamine. This process, known as degranulation, can lead to symptoms such as itching, hives, flushing, headaches, and even anaphylaxis in severe cases.
- Symptom Fluctuations: People with MCAS often report that their symptoms worsen during periods of low barometric pressure, such as before a storm or during rapid weather changes. This can be due to the mast cells’ heightened reactivity to environmental stressors.
Effects on Dysautonomia:
- Blood Pressure Regulation: The autonomic nervous system, which is impaired in dysautonomia, helps regulate blood pressure in response to environmental changes. When barometric pressure drops, the body’s ability to maintain stable blood pressure can be disrupted, leading to dizziness, lightheadedness, and fainting.
- Headaches and Migraines: Low barometric pressure is a known trigger for headaches and migraines, which are common in people with dysautonomia. This can occur because pressure changes affect the blood vessels in the brain and the body’s pain receptors.
- Increased Fatigue and Weakness: Rapid changes in barometric pressure can lead to increased fatigue and a sense of weakness, as the body struggles to adapt to the environmental shift. This is particularly challenging for those with dysautonomia, where energy levels and autonomic stability are already compromised.
Coping Strategies:
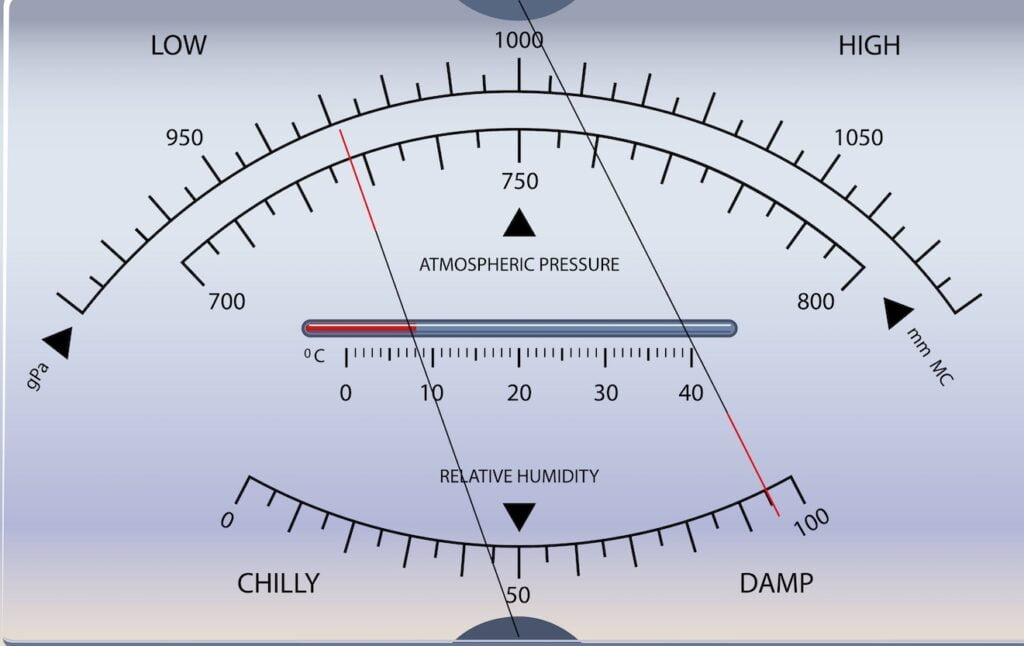
- Track Weather Patterns: Knowing when barometric pressure is expected to change can help you prepare for potential symptom flare-ups.
- Controlled Environment: Staying indoors in a stable environment where you can control temperature and humidity might help reduce the impact of barometric pressure changes.
- Manage Stress: Since stress can exacerbate both conditions, having stress-relief strategies in place (like deep breathing, meditation, or light exercise) can be helpful.
- Symptom Management: For MCAS patients, having antihistamines or other prescribed medications readily available during weather changes can help manage sudden symptoms. For dysautonomia, staying hydrated and possibly increasing salt intake (if advised by a healthcare provider) can help manage blood pressure changes.
Both conditions require a personalized approach, so discussing these strategies with a healthcare provider is essential for managing symptoms effectively.